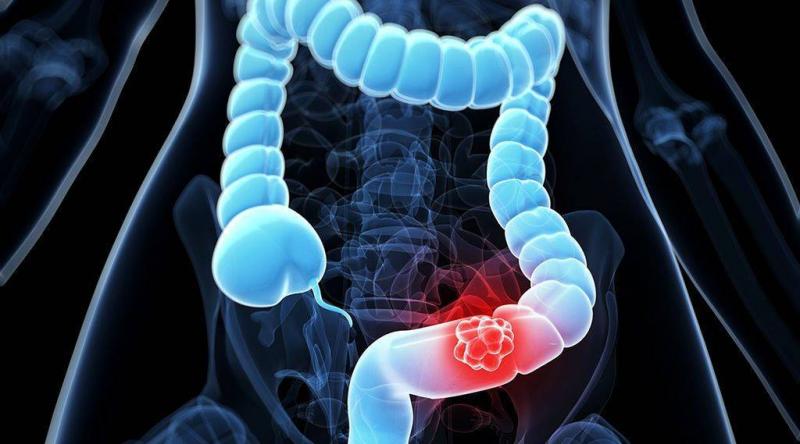
Researchers say that having a colonoscopy as soon as possible after abnormal stool test results can reduce the risk of developing colon cancer and dying from it. In a new study, researchers analyzed data from over 200,000 American veterans aged 50 to 75 who underwent a fecal immunochemical test (FIT) and a fecal occult blood test (FOBT). Both tests are commonly used to screen for blood in the stool.
Abnormal results in these tests should be followed by a colonoscopy to check for cancerous colon tumors, whether benign or malignant. The study authors found that patients who underwent a colonoscopy more than 13 months after an abnormal stool blood test were 1.3 times more likely to develop colon cancer compared to those who had a colonoscopy three months after the stool test results. Additionally, the risk of advanced colon cancer at diagnosis was 1.7 times higher among patients who underwent a colonoscopy more than 16 months after an abnormal stool blood test, according to researchers from the Veterans Affairs Center who conducted the study.
Furthermore, the study found that the risk of death related to colon cancer was 1.5 times higher when a colonoscopy was performed more than 19 months after the appearance of abnormal stool blood test results. The study was published online on February 2 in the American Journal of Gastroenterology. According to the study's author, Dr. Voulasihd Mai, a gastroenterologist at the Veterans Affairs Healthcare Center in Los Angeles, and his colleagues: "The results of this study expand the current knowledge about the clinical implications of the time patients take to undergo a colonoscopy following abnormal stool blood tests, and this study should encourage further efforts to address the barriers preventing some from undergoing colonoscopy."
The study's authors noted that colon cancer, excluding skin cancers, is the third most common type of cancer in the United States, but it is also one of the most preventable types of cancer since early detection and removal of cancerous polyps can significantly reduce the risk of cancer and related deaths. Moreover, researchers indicated that "currently, there is no national policy or standard for the clinically acceptable interval between abnormal stool blood test results and diagnostic colonoscopy, leading to significant variability in the timing of colonoscopy in practice and among healthcare settings. However, a recommended time interval that is relatively long can contribute to the progression of polyps and the staged growth of colon and rectal cancer, risking the need for more aggressive treatment, as well as decreasing the effectiveness of those treatments over time."