British scientists have developed a new treatment called CAR T-cell therapy that can fight cancer using engineered patient cells, allowing them to remain in the body to prevent cancer recurrence. The researchers conducted trials on numerous patients who had exhausted all other options and were near death, yielding remarkable results. During the trials, all signs of cancer disappeared in over 80% of patients with acute lymphoblastic leukemia, the most common cancer in children, after receiving CAR T-cells. The treatment is also being tested in several other blood cancers, such as multiple myeloma, non-Hodgkin lymphoma, and chronic lymphocytic leukemia.
Dr. Andrew Furness, an oncology consultant at the Royal Marsden Hospital in London, stated that the current applications of CAR T-cell therapy are "just the tip of the iceberg," as doctors and scientists are tirelessly working to expand its reach to more patients. CAR T-cell therapy (or chimeric antigen receptor T-cell therapy) is a form of immunotherapy that harnesses the patient's immune system to fight the disease.
The new treatment works by extracting immune cells known as T-cells to seek out and destroy cancer cells. The process of making the engineered T-cells is lengthy, complex, and costly; it begins by connecting the patient to a machine resembling a dialysis machine, which takes a blood sample, separates the patient's own T-cells, and returns the rest of the blood to the body. The machine repeats this process until 200 milliliters of T-cells are collected, which can take up to six hours. These T-cells are then designed in the laboratory to track and destroy the patient's cancer.
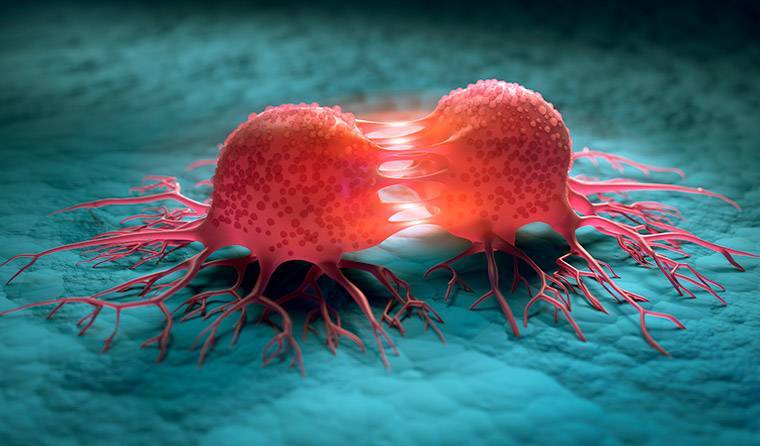
This is done using an inactivated virus to introduce genetic material that instructs the cells to produce a protein called chimeric antigen receptor (CAR) that recognizes a specific protein on the patient's cancer cells. Certain cancers overproduce specific proteins; for example, acute lymphoblastic leukemia (ALL) produces a lot of CD19 proteins, so T-cells are designed for all patients to target this protein. The hypercharged T-cells are then multiplied in the lab before 200 million cells are infused back into the patient via a drip, which takes only two minutes. The cells must establish themselves and kill the cancer cells containing the protein that the T-cells are designed to recognize. Interestingly, CAR T-cells must remain in the body as a "living drug" to prevent cancer from returning.
The entire process costs about $300,000 per patient, starting from the T-cell collection to the infusion of engineered cells back into the patient. Approximately 600 patients, mostly children, have been treated using this new method in the UK. Dr. Emma Nicholson, a hematology consultant at the Royal Marsden Hospital, mentioned that CAR T-cells are likely to be licensed for many other blood cancers within the next two years, according to reports from the Daily Mail.